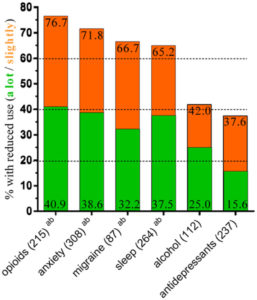
In case you haven’t heard, there is an opioid epidemic in the United States. The phenomenon is not driven by the use of illegal substances, rather it is caused in part by the overprescription of opioid based painkillers, such as Oxycontin. Exploratory studies have suggested that patients with access to medical cannabis reduce their intake of painkillers and hence potentially could help to tame the epidemic. Dose of Science takes a closer look.